Is Behavioral Health the Same as Mental Health – Break down the confusion!
Understanding the language used in health care is crucial—especially when it comes to mental and behavioral health. These terms are often used interchangeably in media, policy, and even clinical settings, which can lead to confusion. Are behavioral health and mental health really the same thing? Or are there subtle but important differences?
This article will explore these two concepts in depth, examining where they overlap, where they diverge, and why distinguishing between them matters—for patients, providers, and policymakers.
What Is Mental Health?
Mental health refers specifically to a person’s emotional, psychological, and cognitive well-being. It encompasses how individuals think, feel, and behave, and also how they handle stress, relate to others, and make choices. Mental health is a foundational element of overall health and is influenced by a range of factors, including:
- Biological factors (e.g., genetics, brain chemistry)
- Life experiences (e.g., trauma, abuse, neglect)
- Family history of mental health problems
The World Health Organization (WHO) defines mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to contribute to his or her community.”
Common mental health disorders include:
- Depression
- Anxiety disorders
- Bipolar disorder
- Schizophrenia
- Post-traumatic stress disorder (PTSD)
- Obsessive-compulsive disorder (OCD)
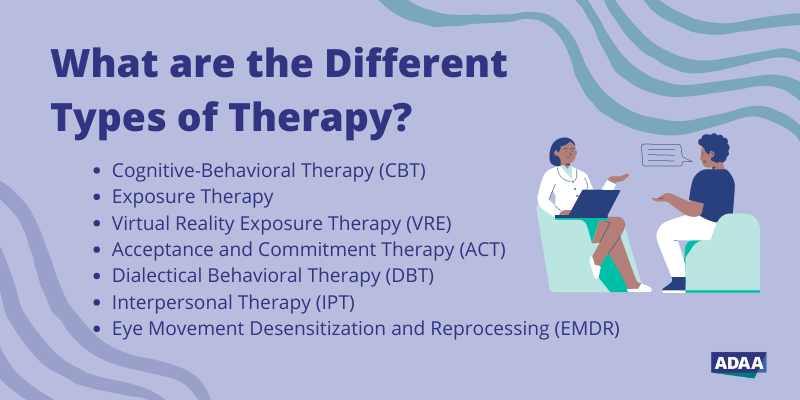
Mental health care typically includes therapy, medication, counseling, and psychiatric support, aiming to treat or manage these conditions and improve the individual’s quality of life.
What Is Behavioral Health?
Behavioral health is a broader term that encompasses mental health but also includes behaviors that impact physical well-being. Behavioral health considers how habits, behaviors, and actions affect both mental and physical health.
The term emerged in public health and clinical psychology to address the relationship between behavior and overall wellness. Behavioral health includes:
- Mental health disorders (e.g., depression, schizophrenia)
- Substance use disorders (e.g., alcohol or drug addiction)
- Eating disorders
- Smoking cessation
- Obesity and weight management
- Chronic illness management (e.g., diabetes, hypertension)
In this context, a behavioral health provider might not only treat mental illness but also help a patient manage behavioral factors contributing to chronic physical conditions. For example, cognitive behavioral therapy (CBT) may be used for both depression and weight loss by addressing underlying thought patterns and behaviors.
Also Read: Does Health Insurance Cover Car Accidents – A Protect Your Finances!
Key Differences Between Behavioral Health and Mental Health
While they are closely related and often overlap, there are important differences between behavioral health and mental health that help explain why the distinction matters.
| Feature | Mental Health | Behavioral Health |
| Scope | Narrower focus on emotional, psychological, and cognitive well-being | Broader scope, includes mental health and behaviors affecting physical health |
| Examples | Depression, anxiety, bipolar disorder | Mental illness, substance use, eating disorders, chronic disease behavior management |
| Providers | Psychiatrists, psychologists, therapists | Includes above, plus social workers, addiction counselors, case managers |
| Treatment focus | Emotional regulation, mood, thinking | Behavioral change, habits, lifestyle impact |
| Origin | Psychiatry, psychology | Public health, clinical psychology |
In Summary:
- Mental health is a subset of behavioral health.
- Behavioral health includes not only mental illness but also behavioral patterns like substance use, eating habits, and adherence to treatment for medical conditions.
Why the Confusion?
There are several reasons why the terms are often used interchangeably:
1. Historical Overlap
Mental health used to be the dominant term in discussions about psychological care. As healthcare models became more holistic and integrated, the term “behavioral health” became more popular, especially in community health and public policy.
2. Insurance and Policy Terminology
Insurance companies and government programs often group mental and behavioral health under one umbrella. For billing and coding purposes, they may not differentiate between the two, further blurring the lines.
3. Clinical Practice
Many professionals, such as counselors, therapists, and social workers, deal with both mental and behavioral issues, using an integrated approach. This reinforces the perception that the two terms are synonymous.
4. Public Perception
To the general public, the differences between behavioral and mental health are not obvious. Media coverage and marketing materials from healthcare providers frequently use them as if they mean the same thing.
Why the Distinction Matters?
While it may seem like a semantic issue, understanding the distinction between behavioral health and mental health can have practical and clinical implications.
1. Tailored Treatment
Mental health treatment may require different modalities (e.g., psychiatric medications, talk therapy) than behavioral interventions (e.g., habit retraining, motivational interviewing). Knowing the difference can ensure patients receive appropriate care.
2. Better Outcomes for Chronic Illness
Behavioral health strategies are essential in treating chronic diseases. For example, patients with diabetes benefit from behavioral health approaches that help them adhere to medication schedules, maintain healthy diets, and manage stress.
3. Stigma Reduction
Understanding that behavioral health includes more than just mental illness can help reduce stigma. People may feel more comfortable seeking help for “behavioral health” issues than for “mental health” disorders, especially in cultures where mental illness is highly stigmatized.
4. Workforce Planning
Health systems need to allocate the right mix of providers. Differentiating between mental health professionals (e.g., psychiatrists) and behavioral health professionals (e.g., addiction counselors) helps with strategic staffing and resource distribution.
5. Policy and Funding
Public health initiatives often fund behavioral health programs that include both mental health and behavioral interventions. Clarity in terms helps policymakers allocate funds effectively.
Integrated Care: Bridging Behavioral and Mental Health
Modern healthcare increasingly adopts an integrated care model—combining primary care, behavioral health, and mental health into a single, coordinated system. This model recognizes the interplay between mental and physical health and aims to treat the whole person.
For example:
- A patient with hypertension and depression might benefit from a team approach including a primary care physician, therapist, and health coach.
- Behavioral health professionals help patients develop healthier lifestyles, while mental health specialists address emotional or psychological challenges.
Integrated care is especially important in underserved populations and rural areas, where access to specialized services may be limited.
Common Misconceptions:
Here are a few myths and misunderstandings about behavioral and mental health:
1. “Behavioral health is only about substance abuse.”
False. While substance use disorders are a key part of behavioral health, the field encompasses many other issues, from anxiety to chronic disease self-management.
2. “Mental health doesn’t involve behavior.”
Also false. Mental health conditions often manifest as behavioral changes—like withdrawal, aggression, or risky behaviors. In fact, behavioral therapies are commonly used to treat mental illness.
3. “Only people with disorders need behavioral health support.”
Not true. Behavioral health includes wellness and prevention services aimed at everyone—like stress management programs, wellness coaching, and resilience training.
Real-World Applications:
Understanding the behavioral vs. mental health distinction helps in various settings:
1. Schools
School counselors often work on both behavioral and mental health issues—helping with emotional regulation, while also addressing behavioral problems like attendance or substance use.
2. Workplaces
Employee assistance programs (EAPs) that include behavioral health support can offer broader benefits—helping employees manage stress, quit smoking, or seek help for anxiety or depression.
3. Hospitals
Inpatient units often have behavioral health teams that manage both psychiatric crises and behavior-linked medical issues (like non-adherence to treatment).
FAQ’s:
1. Is behavioral health the same as mental health?
No. Behavioral health is a broader term that includes mental health as well as behaviors that affect overall well-being—such as substance use, eating habits, and lifestyle choices. Mental health specifically refers to emotional, psychological, and cognitive functioning.
2. Can behavioral health providers treat mental illness?
Yes. Many behavioral health providers, such as therapists and counselors, are trained to treat mental illnesses. Some also specialize in modifying harmful behaviors that impact both mental and physical health.
3. Does insurance differentiate between the two?
Not usually. Many health insurance plans group behavioral and mental health together, although specific services may be billed differently depending on the provider and diagnosis.
4. Can someone have behavioral health issues without having a mental illness?
Yes. A person might struggle with behaviors that affect their physical health—such as poor sleep habits or substance misuse—without meeting the criteria for a mental illness.
Conclusion:
So, is behavioral health the same as mental health? Not exactly. While mental health is a crucial component of behavioral health, the latter represents a broader, more inclusive concept that addresses how behavior influences overall well-being—mental, physical, and emotional.
Read More: